Post-acute care and (long-term) outcome research | Repair
Beside prevention, early diagnosis, and rapid treatment, mid- and long-term care of sepsis survivors eminently impact overall outcome and quality of life of patients suffering from sepsis. Whereas recent data show that sepsis-related mortality in ICUs and hospitals has steadily decreased over the last decade, detailed epidemiological data on sepsis morbidity in the mid- and long-term are lacking. Despite the high clinical relevance, biological mechanisms causing characteristic disease symptoms of patients in the long-term outcome are only rudimentarily understood and treatment options are missing. The lowered sepsis-related mortality has resulted in a larger number of patients and their relatives, who face mid- and long-term consequences of sepsis, thus leading to an increasing burden of disease, which is also becoming continuously more important in public health care. This research area addresses current knowledge gaps and medical need regarding mid- and long-term consequences of sepsis.
The core of this research area consists of three clinical trials and two translational projects:
E
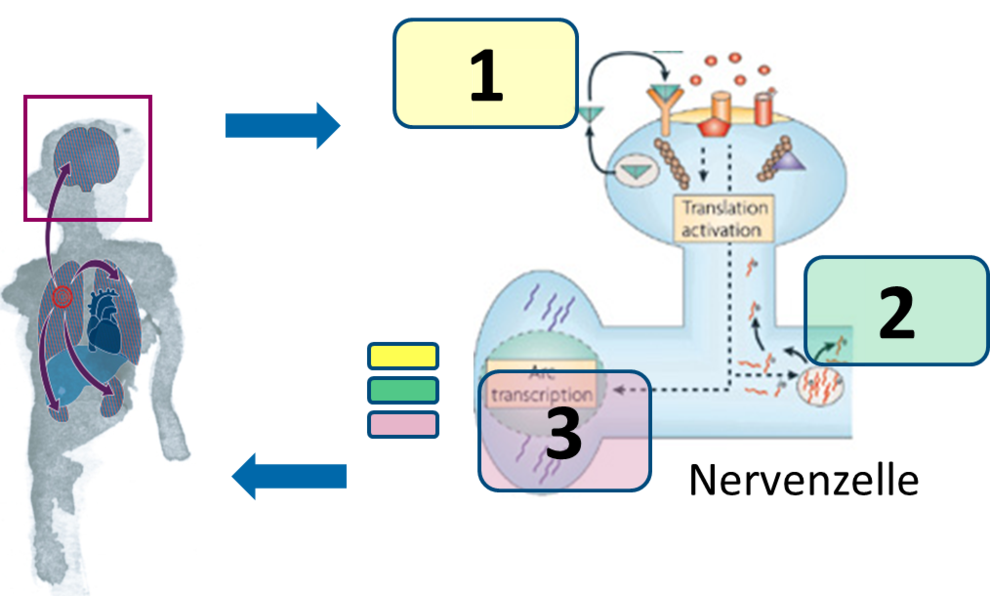
EncRescuePathomechanisms and novel treatment strategies of sepsis-induced cognitive dysfunction
Long-term cognitive dysfunction is a common problem after surviving sepsis. Symptoms include deficits in memory and learning as well as in executive functions. These deficits may last for years or even be irreversible. Neurocognitive dysfunction after sepsis is severe and highly impairing, affecting patients but also families and caregivers. With medical progress, the number of critical ill patients and survivors of severe sepsis in intensive care units increases making long-term cognitive dysfunction to a growing public health problem. In large clinical studies up to 70% of critical ill patients have persistent neurocognitive deficits at hospital discharge and 45% continue to have neurocognitive dysfunction after one year. A recent study demonstrates that about one third of survivors at one year after discharge have persistent cognitive deficits similar to mild Alzheimer’s disease.
In contrast to the high prevalence and clinical relevance, the pathophysiology underlying cognitive deficits after severe sepsis is largely unknown. Causative therapeutic options are missing. In preliminary studies to EncRescue we established a mouse model for severe sepsis and evaluation of long-term cognitive dysfunction. We found characteristic phenotypic changes, deficits in neuronal transmission, and specific neurochemical changes in the brain of these animals. Now we aim towards development of therapeutic regimes that are target-directed and interfere with pathophysiological processes in the development and maintenance of neurocognitive dysfunction. In EncRescue we will investigate direct measures to influence pathogenic gene regulation in the brain. In a more translational approach we will also test pharmacological interventions that may open new possibilities for therapeutic approaches in patients.
I
IcosmosQuality improvement in infection control and sepsis management in model regions

Sepsis – major indicator for quality improvement in healthcare
- Sepsis is a frequent condition in health care with rising numbers, considerable mortality, and relevant strain on resources.
- Quality initiatives in several countries were able to lower sepsis-related mortality by 10 – 30%
ICOSMOS – sustainable improvements in health care
- Individualized quality reports – measuring your own quality and benchmarking with other participating hospitals as well as the “German average”.
- Support in trainings towards a more adequate coding
- Support in establishing and enhancing a sepsis quality management
- Supply of training- and information-material for seminars and training
- Optional participation in external peer-reviews
ICOSMOS – little effort and costs, high security and confidentiality
- No extra documentation needed – all analyses are based on routinely collected data (§21 KHEntgG)
- All costs for data management and quality reports are covered by funding (BMBF)
- Data analyses an management in cooperation with 3M Health Information Systems (3M HIS), Germany, an experienced long-term partner in the field of quality management and routine data for other national and international quality intiatives (e.g. “IQM”).
- Warranty of privacy and confidentiality – no publication of hospital related data by the study coordination team, no access to hospital related data for any other Jena University Hospital personnel than the study coordination team.
- Small annual participation fee
M
Mid-German Sepsis CohortMSC

The Mid-German Sepsis Cohort (MSC) is planned as the world's largest cohort study, which will comprehensively document the functional, cognitive and psychological effects and changes in quality of life after treatment of severe sepsis in the intensive care unit (ICU).
The MSC will have a recruitment period of 3 years and an initially funded follow-up period of one year; a 5 year follow-up is intended. A total of five study centers are involved in the recruitment. Included are patients with severe sepsis / septic shock who have been treated at an ICU and who are at least 18 years at discharge and for which there is a consent form. There are no specific exclusion criteria. Patients will be followed up at regular intervals after discharge from the ICU as long as possible. In addition to general characteristics of patients and their intensive care, functional consequences are a primary interest of the MSC; they are summarized as "activities of daily living" or "instrumental activities of daily living" (e.g. running, dressing, washing). Furthermore, other patient-relevant outcomes such as health-related quality of life, cognitive impairments, post-traumatic stress, anxiety and depression, and neuromuscular deficits, pain, sleep disorders, weight and the resumption of work are assessed. The MSC will also work as a support platform for the participating patients and their families. Ultimately, the generated results will help to develop specific, adapted rehabilitation programs.
R
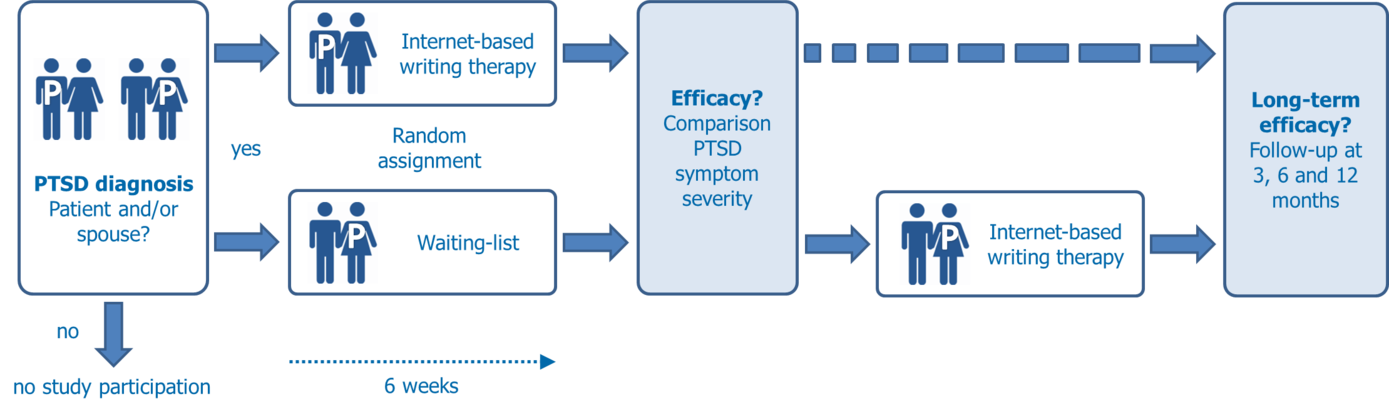
RepairReducing posttraumatic stress after severe sepsis in patients and their spouses

Mental disorders like post-traumatic stress disorder (PTSD) are common consequences of intensive care of severe sepsis and do not only affect patients but also spouses.
Primary aim of the project is to evaluate the efficacy and safety of an internet-based therapy of post-traumatic stress disorder in patients who survived a severe sepsis and their spouses.
Study participants will be randomly assigned either to a therapy group or a waiting-list. Patients of the therapy group attend a therapist-assisted, internet-based writing therapy to treat PTSD consisting of two weekly writing tasks over a six-week period (11 essays in total). The waiting-list serves as a control group against spontaneous remission and receives treatment after the waiting period of 6 weeks.
Adult patients after severe sepsis with an ICU stay of 5 days+ or spouses of patients will be included if they are diagnosed with PTSD that is associated with ICU stay for treatment of sepsis. Exclusion criteria are living alone, acute psychosis, suicidal intentions, severely depressed mood, use of neuroleptics, and concurrent psychotherapeutic treatment.
Primary efficacy endpoint is symptom severity of posttraumatic stress at the end of treatment. Further outcomes are remission of PTSD, depression, anxiety, somatization, marital satisfaction, health related quality of life, and therapy dropout. Follow-up assessment to evaluate long-term efficacy will be 3, 6 and 12 months after treatment.
Altogether, 98 patients and their spouses will be included. The study is scheduled for 36 months, with a recruiting period of 24 months.
Further information (in German) for people interessed or affected is available at www.zweileben.net
S
SepSysSystems Biology of Sepsis
Our aim is to develop systems biology models to
- spot molecular players and pathways relevant for the unbound inflammatory response in order to
- decipher molecular mechanisms leading to
- the identification of biomarkers for early diagnosis, and to
- the identification of specific targets for therapy.
For this, we will develop new methods and integrate omics datasets of septic patients’ blood and of several tissues of animal models, such as gene expression profiles, but also genomics, metabolomics, proteomics data and next generation sequencing data. We will develop models to observe regulation of cellular signaling and metabolism, also within different organs. We will analyze the impact of genetic variants on the clinical course of sepsis patients. In particular, loss-of-function gene variants will be associated with unexpectedly good disease progression, which will lead to potential drug targets for therapy. Methodologically, we will develop gene regulatory models for signaling, regulation, and metabolism and interconnect them to understand the pathologic regulation of central pathways linking receptors, the mediating signaling pathways and in particular regulation of metabolism of the affected cells. In addition, we will set up dependency models, linking the regulation of the involved organs, to find crucial players mediating these signals. These players will serve for improved drug target predictions. The predictions of our models will be the basis for experimental validation and follow-up of CSCC cooperation partners.





